SAFETY SUMMARY
Warnings -
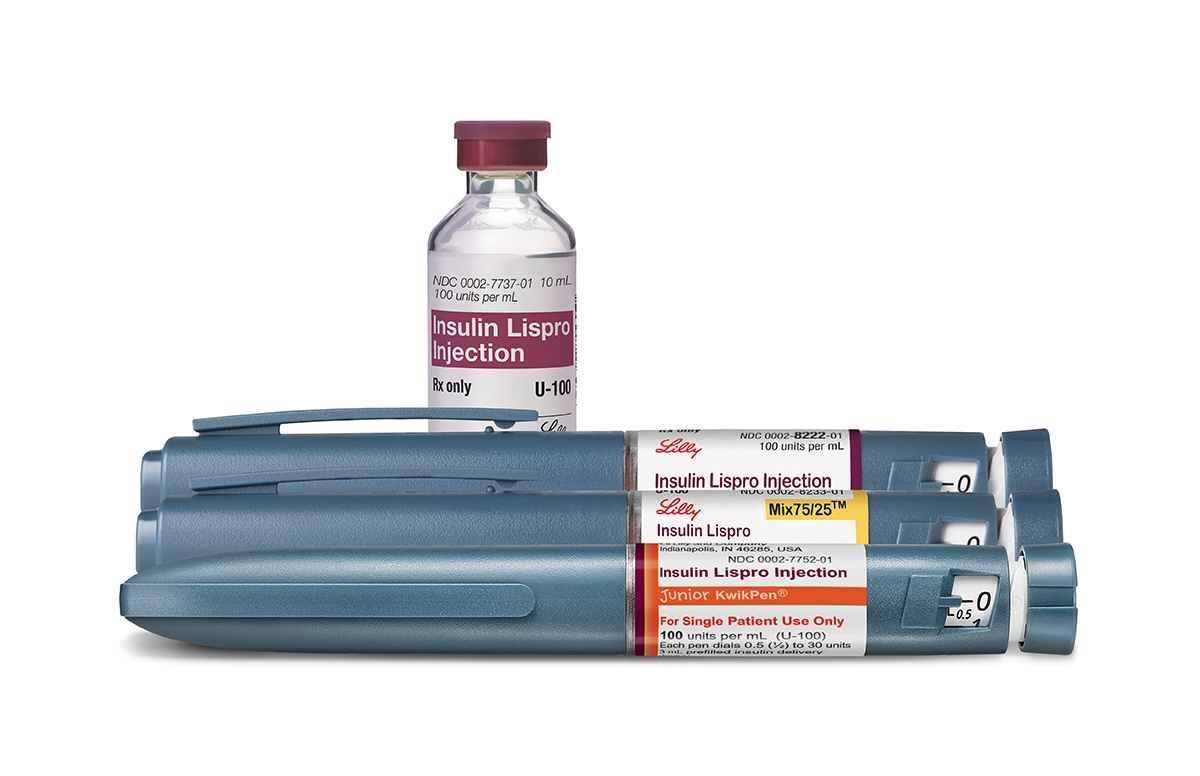
Do not take Humalog, Insulin Lispro Injection, Humalog Mix50/50, Humalog Mix75/25, or Insulin Lispro Protamine and Insulin Lispro Injectable Suspension Mix75/25 if you have:
- symptoms of low blood sugar (hypoglycemia)
- an allergy to insulin lispro products or any of their ingredients.
Do not reuse needles or share your insulin injection supplies with other people. This includes your:
- prefilled pen for use by a single patient
- cartridges
- reusable pen that works with Lilly 3mL cartridges
- needles
- syringes
You or the other person can get a serious infection. This can happen even if you change the needle.
Do not change the type of insulin you take or your dose, unless your doctor tells you to. This could cause low or high blood sugar, which could be serious.
Do not use a syringe to remove Humalog from your prefilled pen. This can cause you to take too much insulin. Taking too much insulin can lead to severe low blood sugar. This may result in seizures or death.
Humalog, Insulin Lispro Injection, Humalog Mix50/50, Humalog Mix75/25, and Insulin Lispro Protamine and Insulin Lispro Injectable Suspension Mix75/25 may cause serious side effects. Some of these can lead to death. The possible serious side effects are:
- Low blood sugar. This can cause:
If you are at risk of having severely low blood sugar, your doctor may prescribe a glucagon rescue medication. These are used when your blood sugar becomes too low and you are unable to take sugar by mouth. Glucagon helps your body release sugar into your bloodstream.
- dizziness or light-headedness
- headache
- shakiness
- irritability
- sweating
- blurred vision
- fast heartbeat
- mood change
- confusion
- slurred speech
- anxiety
- hunger
- Severe allergic reaction.
Get emergency help right away if you have:- a rash over your whole body
- sweating
- extreme drowsiness
- swelling of your face, tongue, or throat
- trouble breathing
- a faint feeling
- dizziness
- a fast heartbeat
- shortness of breath
- confusion
- Low potassium in your blood. This can lead to severe breathing problems, irregular heartbeat, and death.
- Heart failure. Taking diabetes pills called thiazolidinediones (thIE-uh-zOH-li-dEEn-dIE-OHns), or "TZDs," with insulin lispro products may cause heart failure in some people. This includes people who do not have any heart problems. If you have heart failure, it may get worse if you take TZDs with these insulin lispro products. Tell your doctor if you have any new symptoms of heart failure, or if they get worse. Some symptoms of heart failure include: shortness of breath, swelling of ankles and feet, and sudden weight gain. Your doctor may need to change or stop treatment with TZDs and your insulin lispro product.
- High blood sugar and ketoacidosis. You can have these serious problems when your insulin pump or infusion set stops working. They can also happen if your insulin is no longer effective. For these reasons, always keep extra insulin injection supplies with you.
Common side effects
The most common side effects of Humalog, Insulin Lispro Injection, Humalog Mix50/50, Humalog Mix75/25, and Insulin Lispro Protamine and Insulin Lispro Injectable Suspension Mix75/25 are:
- low blood sugar
- reactions where you have injected insulin
- swelling of your hands or feet
- itching
- allergic reactions
- changes in fat tissue where you have injected insulin
- weight gain
- rash
These are not all of the possible side effects. Tell your doctor if you have any side effects. You can report side effects at 1-800-FDA-1088 or www.fda.gov/medwatch.
Before using
Talk with your doctor about low blood sugar and how to manage it. Also tell your doctor:
- about all of the medicines you take, including over-the-counter medicines, vitamins, and herbal supplements.
- about any other prescription medicines you take, especially ones called TZDs.
- about all of your medical conditions, including if you have heart failure or other heart, liver, or kidney problems.
- if you are pregnant, breastfeeding, or plan to become pregnant or breastfeed.
How to take
Read the Instructions for Use that come with your Humalog, Insulin Lispro Injection, Humalog Mix50/50, Humalog Mix75/25, or Insulin Lispro Protamine and Insulin Lispro Injectable Suspension Mix75/25. Be sure to take your insulin lispro product and check your blood sugar levels exactly as your doctor tells you to. Your doctor may tell you to change your dose because of illness, increased stress, or changes in your weight, diet, or physical activity level. He or she may also tell you to change the amount or time of your dose because of other medicines or different types of insulin you take.
Before injecting your insulin lispro product
You can inject your insulin dose yourself, or you can have a trained caregiver inject it for you. Make sure you or your caregiver:
- Check the insulin label before each injection. This will help you make sure that you are taking the correct insulin.
- Use a new needle for each injection. You can get a serious infection or the wrong dose of insulin if you re-use needles.
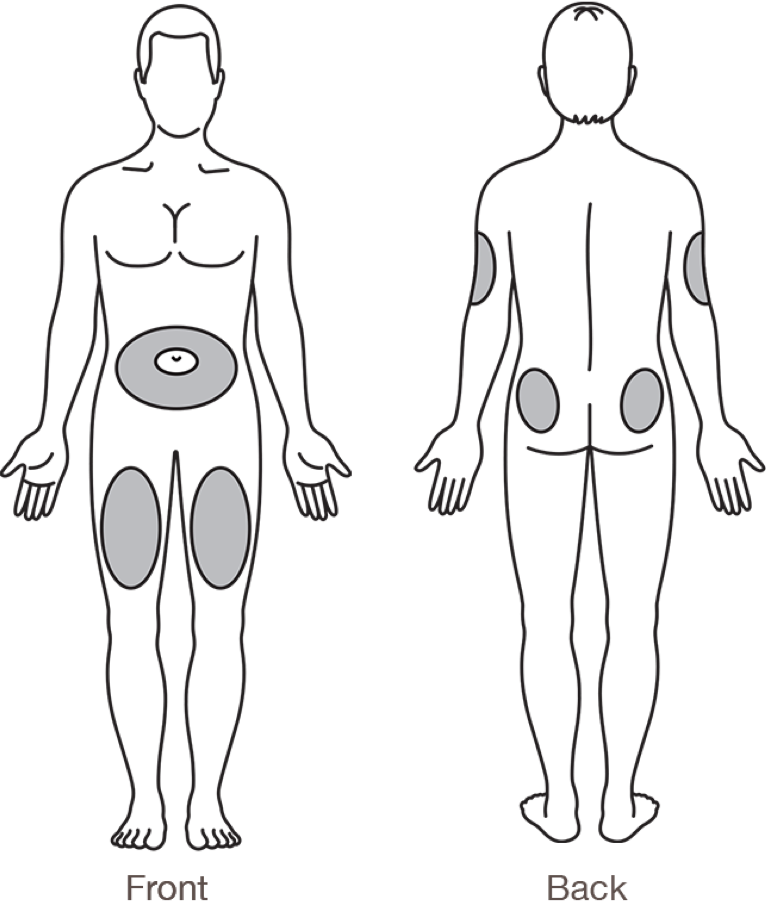
- Change (rotate) where you inject your insulin with each dose. This can reduce your chance of getting pits, lumps, or thickened skin where you inject your insulin. Do not inject your insulin into the exact same spot or where the skin has pits or lumps. Avoid injecting into thickened, tender, bruised, scaly, hard, scarred, or damaged skin.
When you are ready to inject
- If you are taking Humalog or Insulin Lispro Injection, inject it under your skin within 15 minutes before or right after you eat a meal.
- If you are taking Humalog Mix50/50, Humalog Mix75/25, or Insulin Lispro Protamine and Insulin Lispro Injectable Suspension Mix75/25, inject it under your skin within 15 minutes before you eat a meal.
Staying safe while taking your insulin lispro product
To stay safe while taking your insulin, be sure to never inject Humalog U-200, Humalog Mix50/50, Humalog Mix75/25, or Insulin Lispro Protamine and Insulin Lispro Injectable Suspension Mix75/25 in your vein, muscle, or with an insulin pump. Also be sure not to:
- mix Humalog U-200, Humalog Mix50/50, Humalog Mix75/25, or Insulin Lispro Protamine and Insulin Lispro Injectable Suspension Mix75/25 with other insulins or liquids.
- drive or use heavy machinery until you know how your insulin lispro product affects you.
- drink alcohol or use other medicines that contain alcohol when taking your insulin lispro product.
Learn more
Humalog, Humalog Mix50/50, Humalog Mix75/25, Insulin Lispro Protamine and Insulin Lispro Injectable Suspension Mix 75/25 are prescription medicines. For more information, call 1-800-545-5979.
This summary provides basic information about Humalog, Insulin Lispro Injection, Humalog Mix50/50, Humalog Mix75/25, and Insulin Lispro Protamine and Insulin Lispro Injectable Suspension Mix75/25. It does not include all information known about these medicines. Read the information that comes with your prescription each time your prescription is filled. This information does not take the place of talking with your doctor. Be sure to talk to your doctor or other health care provider about your insulin lispro product and how to take it. Your doctor is the best person to help you decide if these medicines are right for you.
HI BOI SP U100 75/25 CON BS 22NOV2023